Have you ever dreamed about being superhero? To have all those amazing abilities: to fly, see through walls, hear everything and a lot of more, just to be able to help someone. Wouldn’t it be great to see someone smiling just because you saved his life? Well, there is one way we could all be superheroes, way we could all save someones life just in a few minutes and all of that without using any superpowers we mentioned till now. All you need is power of Compassion, Charity and power of Love.
1. History
The practice of blood transfusion, that is the transference of blood from the circulation of one individual to that of another for practical therapeutic purposes, is of relatively recent origin. Although it only became a practical possibility during and shortly after the Second World War the concept of ‘transfusion’ has a longer history.The idea though of the theoretical beneficial effects of blood transfusion has been recognised for over three centuries.
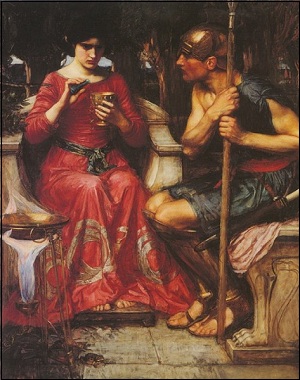
There are many early documented references to the use of blood, for what can be at best described as ‘medicinal’ purposes. One of the first of these relating to a ‘transfusion’ is contained in the seventh book of the Metamorphoses, by Ovid, who wrote in 43BC, describing how (the witch) Medea rejuvenated Jason’s aged father Aeson. In addition to these early mythical writing, there are several noted citations in the Old Testament indirectly bearing on (blood) transfusion. These have a social impact to the present day, relating to the denial of a blood transfusion by certain persons, on religious grounds.It is believed that the ancient kings of Egypt apparently bathed in blood, believing such baths to “… resuscitate the sick and rejuvenate the old and incapacitated”, as well as believing it to be a cure for elephantiasis!
This older history is based on the traditional idea of blood as being the ‘living-force’ of the body. Man must have recognised that loss of blood was frequently associated with weakness and death. This was manifested by Greeks and Romans committing suicide by ‘opening a vein’ (involving cutting their wrists). Blood was recognised as having numerous mysterious properties, including initially that of carrying both the mental and physical characters of its owner. Early attempts at replacing lost blood involved the drinking of blood by the patient. By choice, this was from a young, healthy, fit person or animal. In classical times the Romans and Greeks, as well as bathing in blood, have reportedly drank it. Their spectators also rushed into the arena to drink the blood of dying gladiators. These people did this because they felt that such blood was especially beneficial since the athletes were strong and brave.The legend of the vampire originates from this concept. This somewhat mystical fascination with the properties of blood is to some degree still with us today.
An early recognition of the dangers of the custom of ‘ingestion’ of blood, as well as probably the first rather fanciful description of what could be described as the management of an adverse reaction, is contained in the works of the 13th Century writer Petro de Abano, who wrote: “He who drinks of menstrual blood or that of a leper will be seen to be distracted and lunatic, evil minded and forgetful, and his cure is to drink of daisies powdered and mixed with water of honey, and to bath in tepid water and to copulate with girls according to the law natural, and to play with pretty girls and young boys; and the antidote is to eat serpents whose heads and tails have been cut off with the edge of a palm frond.”
Since most of the ancient and medieval references probably refer to the ingestion of blood, rather than to its infusion, it is in fact difficult to determine when the first authentic attempt at transfusion was actually performed. One of the most frequently quoted candidates for this noteworthy honour is Pope Innocent VIII, Giovanni Cibo, who was reputedly ‘transfused’ some time between 1490 and 1492.On one occasion, after all means to revive the Pope had failed, it is reported that a physician (or mystic) of dubious reputation, named Abraham Meyre, appeared in the court and promised to save the Pope’s life by transfusing him with the blood of young ‘donors’. Apparently, three young 10-year-old shepherd boys were selected as donors and Villari states that the blood of the dying Pope was passed into the veins of one of the boys, “… who gave him his own in exchange”. The process was apparently repeated with the other two boys. All three boys apparently died shortly after the procedure, possibly as a result of air embolism, but there was no change to the Pope’s condition.
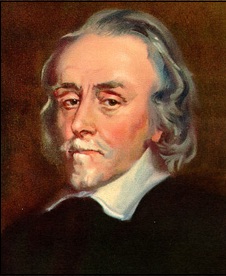
One of the most important discoveries permitting the transfusion of blood was then made, that of the formulation of the theory of the circulation of blood, discovered by William Harvey in 1613. William Harvey was a doctor who identified that that blood flowed through blood vessels in one direction. Up until then, blood was assumed to wash forwards and backwards in the vessels, like the tides of the sea.
In1667. Dr Jean Denys, a young physician on the large staff attached to King Louis XIV, performed numerous dog-to-dog transfusions.On the 15th June 1667, Denys was asked to treat a 15-year-old boy, who had suffered from a fever or many months. Accordingly he was bled to the extent of about three ounces and received in exchange nine ounces of blood from the carotid artery of a lamb. After treatment boy was not having further ill effects. Denys’ second transfusion was performed on a 45-year-old man using a reported 20 ounces of lambs’ blood and described the man as feeling stronger than before the transfusion.
in 1678, an edict from the French parliament ruled transfusion to be criminal act if performed in France. This had repercussions in London where the Royal Society rapidly washed its hands of transfusion as well. Finally, in 1679 the Pope joined the general outcry and also announced a ban on the procedure. As a result, quite understandably, interest in transfusion rapidly waned.
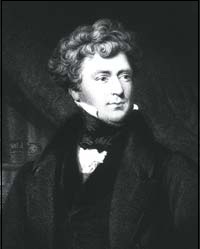
The credit for placing transfusion on a scientific basis and re-awakening interest in its use must be given to James Blundell (1790-1877). James Blundell was a noted physician, physiologist and one of the outstanding obstetricians of his day. He is credited not only with rekindling interests in blood transfusion in the second decade of the 19th century and providing it with a semblance of a national approach, but was the first to transfuse human blood. Many people in fact regard Blundell as the ‘the father of modern blood transfusion’.The first successful transfusion was of a woman who recovered from severe post-partum haemorrhage after receiving eight ounces of blood from Blundell’s assistant during the course of three hours. This case was published in journal ‘The Lancet’ in 1829.James Blundell established, during his interest in transfusion, so many fundamental points that it is difficult to exaggerate the importance of his work in the history of transfusion medicine.
Now we’ll skip few decades because a lot of things happened there but still they haven’t found equipment that would be pronounced safe enough to be used worldwide in further blood transplantations.

During the final quarter of the 19th Century, frustration and discouragement with blood as a transfusion product resulted in a brief period of enthusiasm for the transfusion of milk, which was thought of as a ‘blood substitute’. This form of treatment achieved its greatest popularity in the United States between 1873 and 1880,with the milk of cows, goats and humans being used and they thought about this first because there haven’t jet found way to stop blood coagulation. By 1878, J.H.Britton, also wrote in the New York Medical Record, that transfusion using milk would entirely supersede transfusions of blood! However, by 1880 increasing numbers of adverse reactions associated with the administration of milk led to its general abandonment.
During the latter part of the 19th Century, the Franco-Prussian war was raging in Europe and the possibility of using blood transfusions on the battlefield naturally came to the fore. In 1882, in Paris,Dr J.Roussel, the chief authority at the time reported on a total of sixty successful transfusions performed since 1865. Roussel’s ‘transfuseur’ apparatus was subsequently officially adopted for use by the French Army and apparently used in time of war.
The dangers of infection (both local and systemic) relating to safe transfusion methods started to be resolved when in 1865 Louis Pasteur recognised that bacterial / fungal contamination causes putrefaction and the work of Joseph Lister who in 1867 discovered antiseptics. As a result, the sterilisation of instruments and antiseptic methods began to be introduced.
The discovery (in 1900) of the human ABO blood groups by Dr Karl Landsteiner in Vienna was the major step in understanding that these wrong reactions were in fact due to what is now known to be blood group incompatibility.
Science and technological developments became more and more involved in the development of transfusion during the 20th Century.The development of electrical refrigeration resulted shortly after in the first ‘blood bank’ being set up in Barcelona in 1936.Current voluntary blood donation process together with the sophisticated methods for the collection, storage, processing and testing of blood required by the complex medical and surgical procedures of the present day are a long way from the early beginnings of drinking the blood of gladiators. However, most of the important developments in transfusion medicine have only been achieved in last sixty years.
2. Myths and Facts
Enough about history…

MYTH: You don’t need me. You have plenty of donors.
FACT: Patients need you! Only about 5% of the eligible population takes the time to donate blood. Blood can not be manufactured in the laboratory. The only source for this lifesaving resource is volunteer blood donors. Approximately 32,000 units are used each day in the U.S.
MYTH: I don’t have time to donate blood.
FACT: Donating blood only takes approximately an hour of your time. The majority of that time is spent filling out a medical questionnaire and checking vital signs. The actual donation process takes about 10 minutes.
MYTH: I can’t give blood because I’m afraid of needles.
FACT: Most people do feel a bit of nervousness about blood donation. Most also say after their donation that they’re sorry they waited so long. Blood donation is a momentary discomfort for the donor that can provide a lifetime of a difference for the patient.
MYTH:When there is a requirement, blood can be manufactured.
FACT: Blood is not something that can be manufactured. It can only come from healthy human beings.
MYTH:Blood donation can tell if one is HIV positive.
FACT: HIV antibodies can take months to develop after infection with the virus. Those recently infected may have a negative test result and yet be able to infect others. It is better not to donate blood if at risk of getting HIV or other infections.
MYTH: Blood lasts forever.
FACT: Red blood cells have a shelf life of only 42 days under refrigeration. Platelets last only 5 days. Every day the South Texas Blood & Tissue Center must collect 500 units of blood.
MYTH: People with tattoos and piercings can not be blood donors.
FACT: Donors who have recently received a tattoo may be accepted, provided the procedure was done at a licensed facility in Texas. Donors must provide the name of the licensed business and the city in Texas where the business is located.
MYTH: I can’t give blood because I have seasonal allergies.
FACT: Allergies, even those that need to be controlled by medication, will not prevent you from donating blood.
MYTH:Health deteriorates after donating blood.
FACT: If you are healthy prior to donation, your recovery is complete in a day or two. It is advised to rest a while after donating. Drinking enough liquids replaces the lost fluid within a couple of hours. The body produces new cells faster after a donation. All the RBCs are replaced within 3-4 days and WBCs within 3 weeks.
MYTH:you cannot take part in sports or other physical activities after donating blood.
FACT: Giving blood does not interfere with ability to perform physically. Advice to avoid heavy lifting or strenuous workouts for the rest of the day is given after the donation. You can get back on track the next day.

MYTH: I can’t give blood because I have high blood pressure.
FACT: As long as your blood pressure is below 180 systolic (first number) and 100 diastolic (second number) at the time of your donation, you may give blood. Furthermore, medications that you may be taking for high blood pressure do not disqualify you from donating.
MYTH: All medications and antibiotics defer you from donating blood.
FACT: Taking medications is NOT an automatic deferral. Most are perfectly acceptable. Since there are many different medications, the easiest thing to do is call the Center to ask. Anyone who is currently taking antibiotics for an infection will be deferred until 24 hours after the last dose. Donors unsure of the medication used will be deferred for a 28 day period.
MYTH: HIV or other infections can be contracted from donating blood.
FACT: A clear procedure exists for taking blood from each donor. Sterility is maintained at all steps. A sterile, new needle is used for each donation and is then properly discarded. Use of sterile equipment and technique limits the chance of infection.
MYTH:Age is a deterrent to blood donation.
FACT: Anyone up to the age of 60 who is fit and healthy can give blood.
MYTH:Heavy people are healthier and have more blood to give.
FACT: Being overweight makes people less healthy. Overweight people do not have more blood.

MYTH: I can’t give blood because I have high cholesterol.
FACT: A high cholesterol level does not disqualify you from donating–even if medication is used to control it. In fact, when you donate blood with CBCO you will get a FREE cholesterol screening!
MYTH:I can’t give blood because I had cancer.
FACT: While some types of cancer may disqualify you from donating, there are many circumstances under which you may donate blood after an appropriate waiting period. Please contact CBCO for more information.
MYTH: Diabetics can not donate blood.
FACT: Type II diabetics (non-insulin dependent) are eligible to donate blood provided the diabetes is controlled by diet and/or oral antidiabetic drugs. Diabetics taking injectable insulin may donate blood if they are stabilized and have not changed their insulin dosage within 2 weeks of donating.

MYTH: I can’t give blood because I have epilepsy or seizures.
FACT: Epilepsy or seizures do not disqualify you from donating as long as you have had no seizures for one year.
MYTH:I can’t donate because I’m anemic.
FACT: Your hemoglobin (iron) level will be checked prior to donating blood. As long as levels are normal on the day of donation, you may give.
MYTH:I can’t give blood because I had a flu shot.
FACT: In fact, you may donate blood the same day you receive the vaccination.
MYTH: Being a vegetarian, means that the blood does not have enough iron and cannot be donated.
FACT: Vegetarians can donate blood. The iron needed is taken from body stores and once a balanced diet is maintained is replaced after donation. This usually normally takes a month or so.
James Harrison:Human Blood Donating Perpetuum Mobile
So much about myths and the facts that put all of them on a side. There are many more of them, people are very creative when they need to find a reason not to give blood. But, there is at least One Man who doesn’t care about those myths and here is a few lines about him.

He is James Harrison, An 74 years old Australian man who has been donating his extremely rare kind of blood for 56 years has saved the lives of more than two million babies.James Harrison, 74, has an antibody in his plasma that stops babies dying from Rhesus disease, a form of severe anaemia.He has enabled countless mothers to give birth to healthy babies, including his own daughter, Tracey, who had a healthy son thanks to her father’s blood.Mr Harrison has been giving blood every few weeks since he was 18 years old and has now racked up a total of 984 donations.
When he started donating, his blood was deemed so special his life was insured for one million Australian dollars.He was also nicknamed the “man with the golden arm” or the “man in two million”.His blood has since led to the development of a vaccine called Anti-D.
He said:”I’ve never thought about stopping. Never.” He made a pledge to be a donor aged 14 after undergoing major chest surgery in which he needed 13 litres of blood.”I was in hospital for three months,” he said. “The blood I received saved my life so I made a pledge to give blood when I was 18.”Just after he started donating he was found to have the rare and life-saving antibody in his blood.
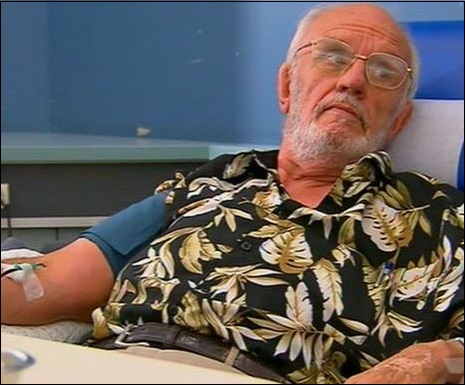
At the time, thousands of babies in Australia were dying each year of Rhesus disease. Other newborns suffered permanent brain damage because of the condition.The disease creates an incompatibility between the mother’s blood and her unborn baby’s blood. It stems from one having Rh-positive blood and the other Rh-negative.After his blood type was discovered, Mr Harrison volunteered to undergo a series of tests to help develop the Anti-D vaccine.
“They insured me for a million dollars so I knew my wife Barbara would be taken care of,” he said.”I wasn’t scared. I was glad to help. I had to sign every form going and basically sign my life away.”Mr Harrison is Rh-negative and was given injections of Rh-positive blood.It was found his plasma could treat the condition and since then it has been given to hundreds of thousands of women.It has also been given to babies after they are born to stop them developing the disease.
It is estimated he has helped save 2.2 million babies so far.